Ahh, the good ol’ mandatory in-service presentation. Yes, it’s something that all PT students get to do for each one of their clinical placements. If you’ve come to the point in your PT journey where you’re on a clinical rotation and you’re in need of some in-service and presentation ideas, this article should hopefully help you out.
This article contains a list of ten in-service topic ideas for multiple different clinical settings as well as why they may be great topics to do an in-service on. If you want to just jump to the list of ideas, scroll down to the section “Ideas and topics for PT student in-service presentations”, but you may find some other great points directly below if you want to read the rest of the article.
HEADS UP: I have two other articles discussing even more in-service ideas in addition to this article. You can check them out here:
Choosing a solid in-service topic should involve a topic that is meaningful and interesting to both you AND the clinical team you’re interning with. Nothing is worse than the combination of having to research and present on a topic that you don’t care about AND having it be a topic that the clinic doesn’t have any interest in either.
Article Overview (Quick links):
Click/tap on any of the topics to instantly jump to that particular topic/section of the article.
These topics are covered in detail below, so keep on reading!
Before you begin to select your in-service topic, it may be helpful to first ask yourself if there will be a preferred presentation style or format based on the preferences or desires of the individuals you may be presenting to (PowerPoint, handout, poster, etc). Most facilities will likely just want a handout but check with your CI.
It is also helpful to get an idea of exactly who you will be presenting to. Sometimes you might just be presenting to your CI, or other times you may be presenting to all the staff PT’s, or you might even be presenting to an inter-professional group (such as a combination of PT’s, OT’s, SLP’s and so on). So, finding out exactly who you’re presenting to can be a great first step to determining what your presentation topic might be.
This can help guide you in your topic selection since knowing your audience can determine the material that is appropriate to present to them (a speech language pathologist who listens to an in-service on some PT-specific interventions might not be very beneficial for them, etc.).
Keep in mind your CI and the facility staff might be rather busy and so a presentation style that is quick and to the point might be best for them. If this were to be the case, providing succinct and easy-to-read handouts might be the way to go.
The best way to figure out what type of presentation would go over best for the staff or the clinic is simply to ask your CI.
If you haven’t done an in-service presentation at any of your clinical rotations yet, I’ll let you in on a little secret: Sometimes your CI and the clinic will be genuinely interested in making you do a presentation, yet other times it will be nothing more than a formality that they make you casually talk about for five minutes as you ride in their Jeep back to the clinic after having taken you out for lunch at Chipotle’s on your last day at the clinic.
CI’s are usually busy individuals with a lot on their plate, so don’t be surprised or upset (maybe you’ll even be relieved) if they don’t take your in-service too seriously or they don’t ask for you to put together anything fancy.
One of my clinicals took the in-service pretty seriously, one took it semi-seriously and two of them didn’t take it seriously at all. That’s just how these things go sometimes.
But I would truly encourage you to take your in-service seriously, if for no other reason than to create a great learning opportunity for yourself. Besides, if you pick a topic that you’re truly interested in, learning more about it and putting it together should actually be an enjoyable process. Whatever information you learn today can only benefit you in the future.
That all being said, let’s dive into it!
The following is a detailed list of ten ideas that could potentially make great in-service topics for one or more of your clinical rotations.
Most ideal clinical setting: Any
What it is: DiSC is a behaviour assessment tool that identifies the behavioural differences within people. It provides a common language that individuals can use as a means to enhance their own understanding of themselves as well as adapt their own communication styles with others. This leads to improved working relationships (therapeutic relationships or others) and helps with identifying and responding to different patient or practitioner styles.
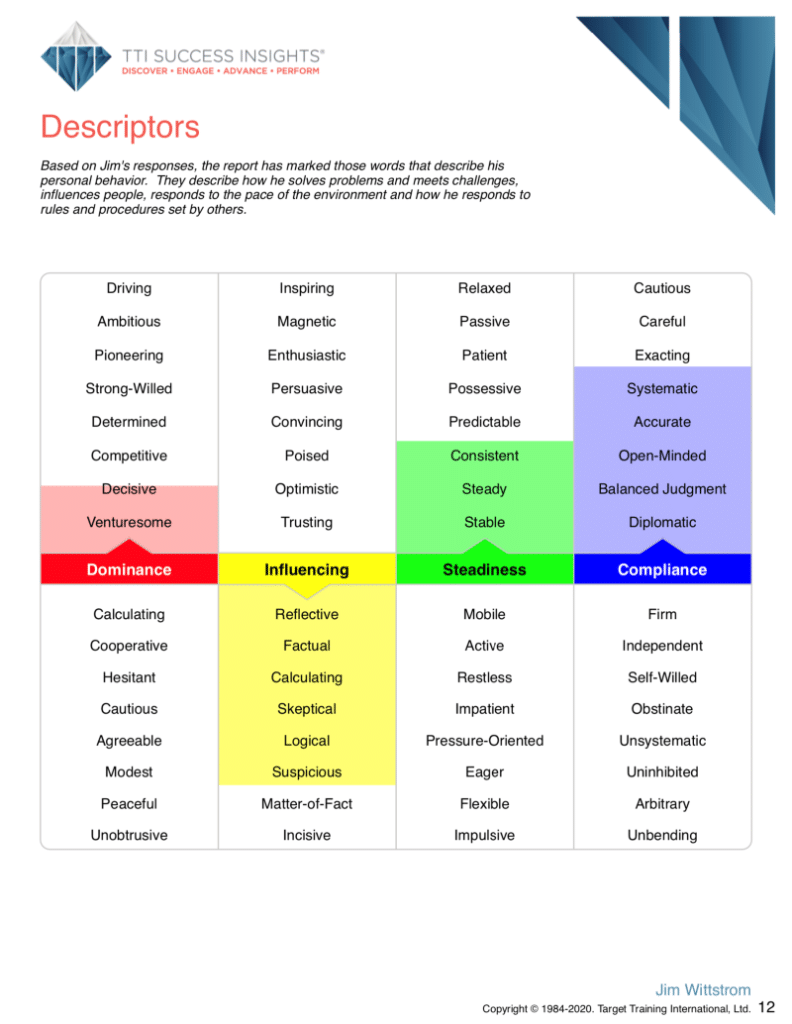
Communication is everything when working with a team and when creating an effective therapeutic relationship with a patient. People (patients and practitioners) have innate differences in the ways they prefer to communicate. Having one communication style trying to communicate with another can oftentimes be like trying to fit a square peg through a round hole.
The DiSC model is what all of us at Tower Physio & Sports Medicine are trained up on, and it has been a game-changer for our patient-practitioner interactions in addition to our team communication.
Most ideal clinical setting: Any
What it is: Motivational interviewing is a counselling-based approach that is designed to help individuals identify and subsequently resolve any feelings of ambivalence they may have regarding making a change in their behavior. This exploration of their feelings fosters behavioural change within the individual.
MI is based on the belief that patients can be at various stages of readiness for change, and that a non-judgmental approach by the clinician involving change talk can draw out motivation within the patient that will help them to change their behaviour.
Physical therapists often work with patients who have a desire to create positive lifestyle changes (become more active, get healthier, etc.) yet experience ambivalence with making their changes.
Having the knowledge and skills to help patients explore and identify their ambivalence (in a non-judgmental manner) can help elicit positive change within these individuals, leading to behavioural change and greater outcomes for health and quality of life.
Most ideal clinical setting: Any
What it is: Cannabidiol (CBD) oil is a type of cannabinoid that is derived from cannabis. Cannabinoids are chemicals that are found in marijuana plants. CBD is distinctly different from the cannabinoid THC, which also comes from marijuana plants and is the chemical that produces the “high” felt when consuming it.
The past few years have seen explosive growth in the use of CBD oil for a variety of health-related reasons. Patients being treated by physical therapists often report great levels of pain reduction when used for this purpose. While also used for other medical conditions such as anxiety reduction or as an anti-epileptic, the effects of CBD oil on pain and pain perception are of special interest to healthcare workers such as us PT’s.
While a high percentage of individuals report very favorable outcomes in pain reduction with CBD oil, science still isn’t entirely certain of how exactly this occurs or for all the conditions it may be beneficial for. An in-service report on types of conditions it may be most favorable for, mechanisms of its purported action and other details pertaining to CBD oil use could be very valuable for PT’s or other healthcare professionals you may be interning with.
Head on over to the ever amazing website examine.com and you could quickly bang out an in-service presentation on CDB based on their scientific findings: https://examine.com/supplements/cbd/
Most ideal clinical setting: Orthopedics
What it is: Blood Flow Restriction therapy involves exercising at relatively low intensities of maximal load while using pressurized cuffs around one or more of the extremities (restricting venous return – but NOT occluding it) in order to elicit a disproportionately favorable outcome of muscle strength and growth as a result.
The basic mechanism occurs by building up a metabolic environment within the blood in the extremities in a way that is similar to high-intensity, high-loading exercises. This buildup of metabolites essentially tricks the brain into thinking this is what has taken place when the cuffs are released and the high concentration of metabolites enters systemic circulation.
I did my PICO topic on LL-BFR and have researched it extensively for the past two years and implement it on my patients within my clinical practice when appropriate. Personally, I am a big proponent of this intervention.

Sidenote: If you’re looking to pick up any BFR cuffs, and you would like to get your own, my recommendation is the BSTRONG system, designed by Dr. Jim Stray-Gundersen, a sports medicine physician. If you would like 10% off of any purchase price of their cuffs or products, I have an affiliation with BSTRONG. Simply use the coupon code “JIMWITTSTROM” at the checkout and you’ll get 10% off!
Head on over to the BSTRONG website to learn more about their system and what sets their cuff apart from other brands.
BFR is gaining serious validation in the academic realms for its efficacy in increasing muscular strength and hypertrophy in populations who are at risk or experiencing sarcopenia, muscular atrophy and musculoskeletal weakness due to orthopedic injury or pathologies such as osteoarthritis of the knee.
There’s some pretty great literature and meta-analyses coming out that shed light on its benefit for healthy as well as pathological populations ranging from youth to elderly. As this intervention continues to gain traction, bringing orthopedic-based PT’s up to speed on this topic could make for a great presentation.
Most ideal clinical setting: Any
What it is: The PMCS is a classification system stemming largely from work done at the Rehabilitation Institute of Chicago. to help differentiate and categorize different types of pain that can occur within the body. This system falls within the general “pain science” category.
The PMCS looks at pain coming from the central nervous system (CNS) and the peripheral nervous system (PNS) and classifies pain types into the following categories:
The book itself is filled with assessment and treatment of different types of pain along with treatment strategies and how to educate patients on what they are experiencing.
If you’re looking to pick up the book, you can grab it on Amazon through this link. (Purchasing through this affiliate link helps to support the costs of running this website at no additional cost to you!)
The field of pain science is continually growing now that we’re learning that pain is more complex than we once believed. Having the ability to accurately categorize pain can be extremely beneficial for clinicians who are attempting to treat chronic pain. Knowing the mechanisms and processes that lead to pain helps the therapist to better understand how that particular type of pain is best treated.
Essentially, not all pain is the same, and so the ability to properly sub-classify pain ensures that the correct or best treatment interventions can be employed for that particular pain source. If you don’t fully understand the source and nature of the pain, your interventions may not be effective, just like trying to pound a screw into a board using a hammer.
Most ideal clinical setting: Orthopedics, chronic pain settings
What it is: You’re likely familiar with the concept of central sensitization, but taking a deeper look at the mechanisms behind it could provide valuable insight not only for yourself but to any co-workers you may choose to do your in-service for.
Central sensitization consists of two hallmark features: Expanded receptor-field density and increased temporal summation. There are actually some simple ways that these phenomena are tested for within literature.
Expanded receptor-field density refers to a focal pain spreading out across a larger area than it would under normal conditions, while increased temporal summation refers to how quickly a constant, minor pain would quickly escalate to an intolerable pain (this is exactly how Chinese water torture works, just in case you were wondering).
While a lot of physical therapists understand the concept of what central sensitization is, many of them are unaware of its hallmark features. Providing an in-service that goes into depth on the mechanisms behind being centrally sensitized could provide valuable insight for those who are looking to understand how to better identify this phenomenon, especially when it comes to identification and proper treatment of the condition.
Most ideal clinical setting: Chronic pain-based settings/any
What it is: Opioid-induced hyperalgesia is a condition experienced by patients using long-term opioid medication in which a paradoxical response to pain is created. The nociceptive system in the patient’s body becomes sensitized from the long-term presence of opioids, leading the patient to experience higher levels of pain from a more sensitive pain-response system.
With the ongoing opioid epidemic in the United States, the ability to educate practitioners and patients on the effects of opioid-induced hyperalgesia could be seen as something that is extremely important.
Practitioners who are aware of and well-versed with the existence, specifics and details of opioid-induced hyperalgesia can help better educate their patients and their loved ones on this phenomenon. They can also increase their awareness towards when or how their patients may be at risk for – or experiencing – opioid-induced hyperalgesia. In short, an understanding of when, how and why this condition occurs can provide a multi-faceted benefit to any practitioners to whom you choose to deliver this in-service topic.
Most ideal clinical setting: Outpatient orthopedics, geriatrics
What it is: Quinolone antibiotics are a class of board-spectrum antibiotics typically used to treat bacterial infections. While they can be used for a variety of different bacterial infections, one of their adverse effects is an increased risk of tendon pathologies, including tendon ruptures.
While many medications carry risks of adverse conditions or side effects, the incidence of increased tendon pathology and rupture when taking fluroquinolone medications is not universally known by all physical therapists.
An in-service focused on the prevalence of tendon pathology occurring with fluroquinolone use, populations most at risk, and other factors pertaining to the use of these antibiotics could be valuable, informative and interesting to physical therapists working in a variety of clinical settings.

Most ideal clinical setting: Orthopedics, integumentary/wound care
What it is: While Low-Level-Laser (or light) therapy is slowly becoming more well-known within the world of physical therapy, Class IV laser therapy is a step above traditional “cold lasers” (which are a class III device). Class IV, by definition, refers to a much higher level of power output (wattage) by the laser device. These lasers emit enough energy that they produce heat and burn the skin if not careful.
Class III and class IV laser serve largely the same purpose for treatment within a PT clinic, but class III is essentially a garden hose for power output while class IV is a fire hose. More power means deeper tissue penetration, more light energy delivered to cells and less time needed during the actual laser treatment.
Laser therapy works off of the phenomenon of photobiomodulation, in which light energy is converted to chemical energy within the cells. Class IV laser is starting to gain some great scientific evidence for its ability to hyper-oxygenate tissue, improve blood flow, and upregulate metabolic activity within cells, promoting quicker and greater tissue recovery, especially compared to less powerful class III lasers.
Our clinic uses the K-Laser Cube, which you can check out on K-Laser’s Website (click this link).

The ability to promote greater and quicker tissue healing for certain pathologies can have great significance for both the patient and the practitioner. With class IV laser therapy being able to deliver light dosages to deeper structures within the body (when compared to class III laser), an in-service on this topic could be a perfect fit.
Providing an in-service that looks at where the evidence is at for different types of injuries being positively affected by class IV laser, how class IV laser works, etc. could be very intriguing for any staff members who are unfamiliar with its mechanisms.
My clinic uses the K-laser Cube, and I’ve seen it work wonders for post-operative wounds, tendinopathic issues and other various conditions. K-laser’s website can point you in the right direction for learning more about the basics of these devices, so be sure to check them out!
Most ideal clinical setting: Orthopedic
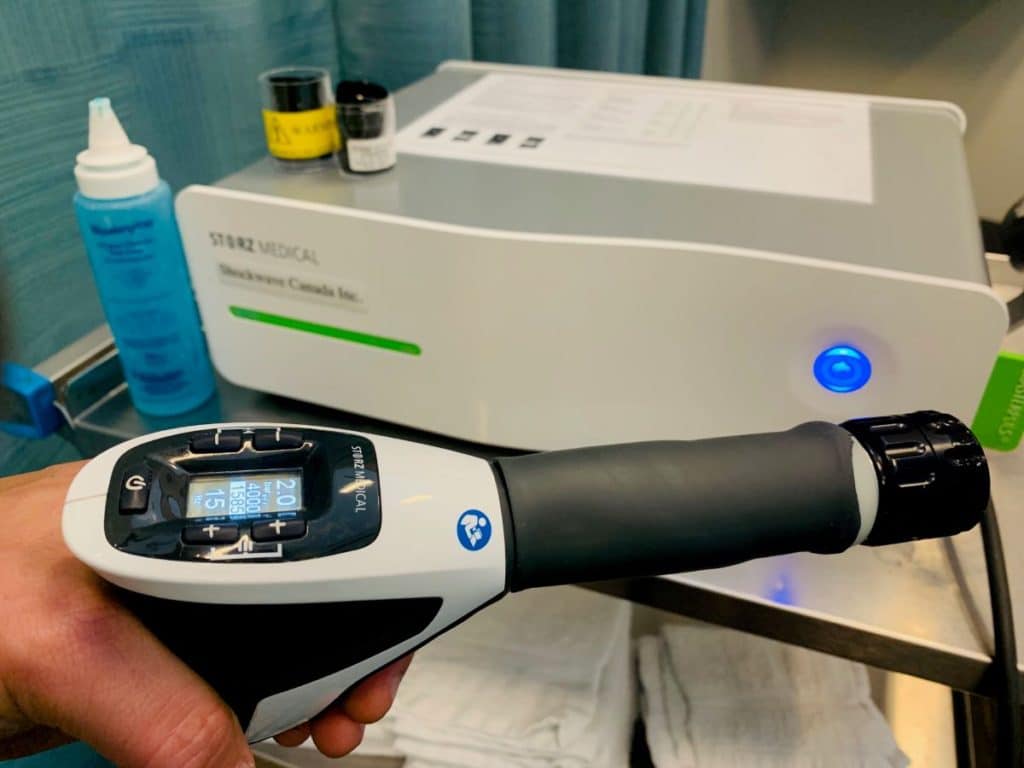
What it is: Extracorporeal Shockwave Therapy (EST) is a treatment modality that has been used in Europe for the past couple of decades while only recently becoming more popular within North America.
EST involves the use of high-powered pressure waves (shockwaves) that are created by having a small metal bullet being rapidly shot down the barrel of a handheld device, which then strikes a ceramic or metal shock plate. This shock plate is pressed up against the patient’s skin, and the resulting pressure waves physically move fluid around within the targeted tissues.
This movement of fluid results in micro cavitations (bubbles) that expand and contract), leading to a cascade of physiologic responses.
EST has been showing very strong effectiveness within literature for treating a variety of conditions often treated by physical therapists.
With the current push for evidence-based treatment within the profession of physical therapy, EST has been proving itself to be a treatment modality that can offer significant benefits for specific pathologies. Physical therapists who deal largely with tendon-based pathologies or fascial restrictions should especially be interested in this modality
Both clinics that I work at use EST as part of the patient’s treatment plan (when appropriate) and I can’t imagine not having it after all the results it has helped produce for my patients. Providing an in-service on the treatment conditions and the effectiveness that EST can provide could be a great topic for clinicians who are unfamiliar with this modality and how effective it can be as an adjunct to a patient’s treatment plan.
When it comes to choosing an in-service topic and the subsequent presentation that goes along with it, make sure that you choose something that benefits both parties; you want to choose a topic that is interesting and relevant for you as well as for those you’re presenting to.
Make sure to choose a presentation style that is best for the needs of the clinic, and don’t be surprised if some of your CI’s don’t take the presentation or in-service all that seriously. Many will, but many won’t.
Hopefully, the ten ideas within this blog post will help spark some ideas for topics that you can consider for your in-service. Needless to say, there are dozens of topics related to each individual topic within this post that you could choose to do a presentation on. It’s an endless world of topics you can choose, and hopefully, after reading this blog post you have either found a topic that will work or at least have a better sense of direction towards where to look in order to find one.
Grind hard. You’ve got this.
Hi! I’m Jim Wittstrom, PT, DPT, CSCS, Pn1.
I am a physical therapist who is passionate about all things pertaining to strength & conditioning, human movement, injury prevention and rehabilitation. I created StrengthResurgence.com in order to help others become stronger and healthier. I also love helping aspiring students and therapists fulfill their dreams of becoming successful in school and within their clinical PT practice. Thanks for checking out my site!